Understanding the Medical Billing Process: A Step-by-Step Tutorial
Introduction to Medical Billing
The medical billing process is a crucial component of healthcare administration, ensuring that healthcare providers are reimbursed for the services they deliver. This intricate process involves several steps, each essential for accurate and timely payment. Whether you're new to the field or seeking to enhance your understanding, this step-by-step tutorial will guide you through the essentials of medical billing.
Step 1: Patient Registration
The process begins with patient registration. This step involves collecting and verifying patient information, such as personal details, insurance information, and medical history. Accurate data collection at this stage is vital for preventing future errors in the billing process.
Insurance Verification
Once patient details are recorded, verifying insurance eligibility is the next step. This entails confirming the patient's coverage with their insurance provider to determine the services covered under their plan. Effective insurance verification can minimize claim denials and ensure smoother billing operations.

Step 2: Medical Coding
Medical coding translates healthcare diagnoses, procedures, and equipment into universal alphanumeric codes. This step is critical as these codes are used for billing purposes. Coders must be meticulous to avoid discrepancies that could lead to claim rejections.
Common Coding Systems
The most common coding systems include ICD (International Classification of Diseases) for diagnoses and CPT (Current Procedural Terminology) for procedures. Accurate coding reflects the services provided and is essential for proper reimbursement.

Step 3: Charge Entry and Claims Submission
After coding, the details are entered into the billing system to generate charges. This step involves inputting all relevant data to create a claim that will be submitted to the insurance company. Ensuring accuracy at this stage is crucial as errors can result in delayed payments.
Claims Submission Methods
Claims can be submitted electronically or through paper claims, though electronic submission is more common due to its efficiency. The claim must comply with insurance guidelines to avoid rejections or denials.
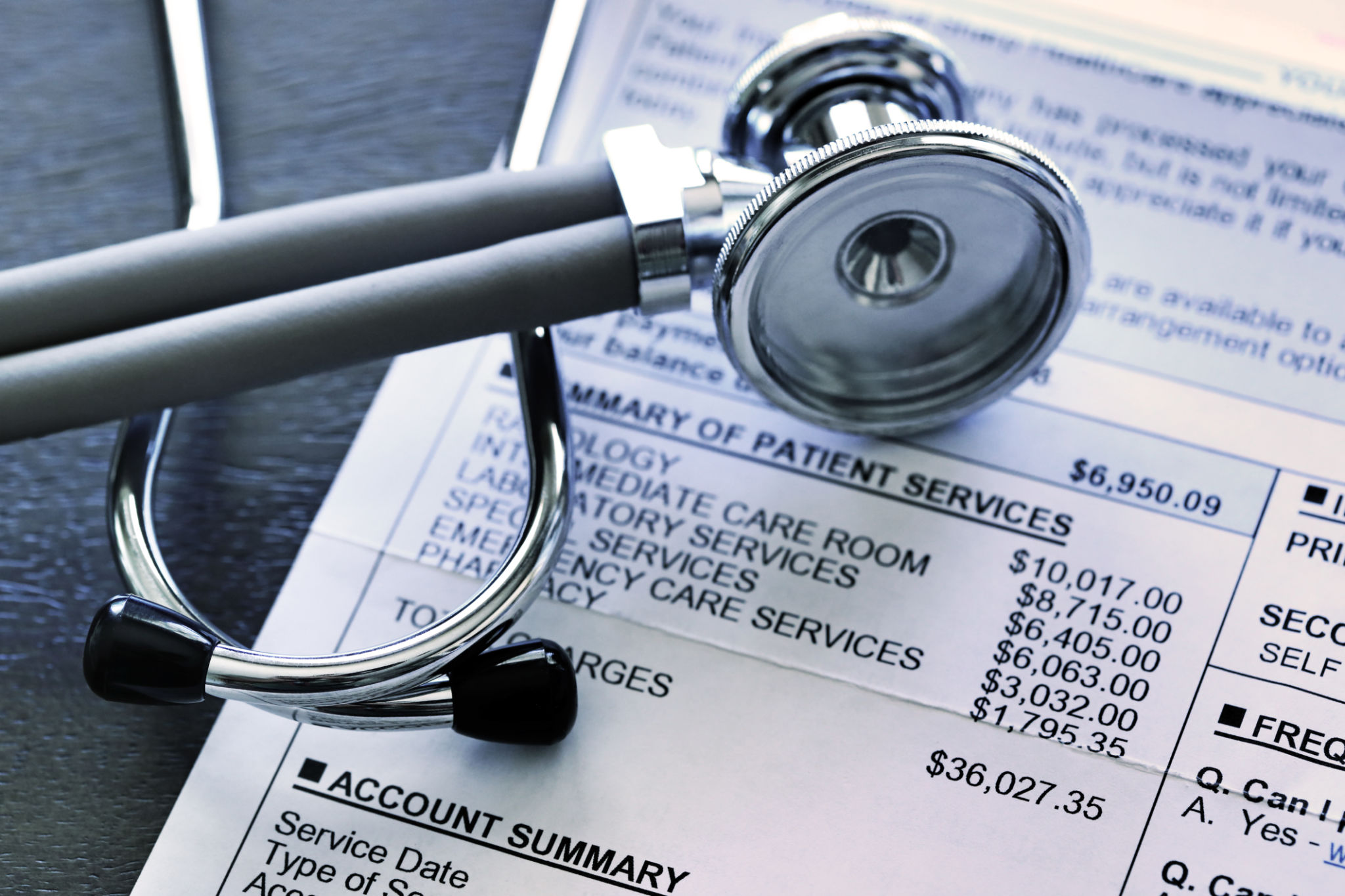
Step 4: Payment Posting
Once the claim is processed, payment posting occurs. This step involves recording payments from insurance companies and patients against the billed amounts. It is vital for maintaining accurate financial records and tracking outstanding balances.

Addressing Payment Discrepancies
Discrepancies between expected and received payments need immediate attention. This may involve reviewing the claim and communicating with the insurance provider for resolution.
Step 5: Managing Denials and Appeals
Inevitably, some claims may be denied or underpaid. Handling these denials involves identifying the reason for denial, correcting any errors, and possibly resubmitting the claim or filing an appeal. A proactive approach can significantly improve recovery rates.
Best Practices for Denial Management
Implementing best practices like thorough documentation, timely follow-ups, and maintaining open communication with insurers can reduce denial rates and enhance the overall efficiency of the billing process.

Conclusion
The medical billing process is multifaceted but understanding each step can greatly enhance its efficiency and accuracy. From patient registration to managing denials, each phase requires attention to detail and a systematic approach. By mastering these steps, healthcare providers can ensure timely payments and focus more on patient care.